Osteochondrosis is a progressive degenerative change affecting the intervertebral discs. Pathology can appear in any part of the spine, but it most often affects the cervical spine.
The problem should not be neglected, because over time the symptoms increase and the pathology itself can result in serious health problems.

What is
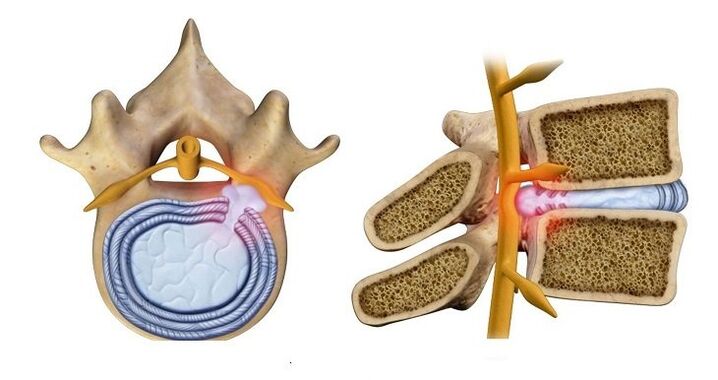
The human spine consists of individual vertebrae, between which there is a special space - the intervertebral disc. It is formed from cartilage tissue and acts as a shock absorber, protecting the bone tissue of the vertebra from wear and tear, while it flattens and wears out.
Normally, such processes occur with the aging of the human body and begin no later than 50-55 years. However, the pathology is becoming younger every year, even in young people (25-30 years old) cases of premature wear of cartilage tissue have been recorded.
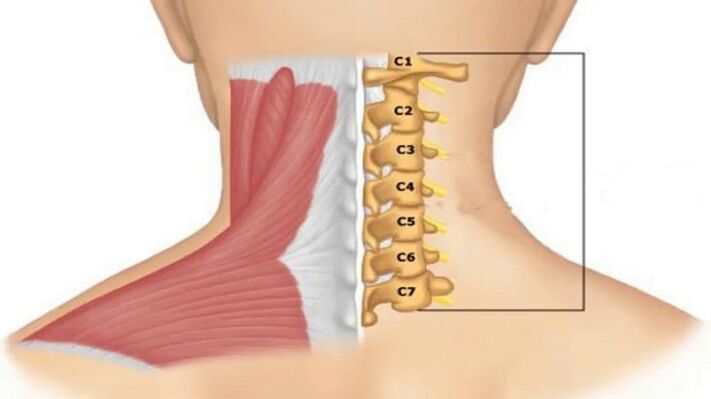
A high percentage of osteochondrosis of the cervical spine, compared to, for example, the spine, is associated with loads on this particular part, caused by the need to keep the skull in an upright position.
The weight of the head of an adult person can reach 3-5 kg: the weight of the bones of the skull is about 1400 g, the weight of the brain is about the same, the mass of blood circulating in the skull is about 500 g.
A feature of the cervical spine is the closer arrangement of the vertebrae and the smaller thickness of the intervertebral discs, which causes complications even with small changes in them.
Reasons for development
Factors contributing to the development of pathological changes in cartilage tissue:
- sedentary lifestyle;
- forced tense postures during work (driving, at the computer);
- overweight;
- state of nervous tension;
- neck injuries;
- muscle weakness.
Neck muscles try to compensate for the load caused by these factors, resulting in their spasm. Blood circulation, cartilage tissue nutrition and metabolic processes are disturbed, which causes changes in its structure.
The following also play a role in premature aging of intervertebral discs:
- hereditary tendency;
- autoimmune diseases that cause degeneration of cartilage tissue;
- congenital pathologies of spinal development.
Stages and symptoms of pathological development
Degenerative changes go through several stages accompanied by certain symptoms:
Stage 1. Symptoms are still practically invisible. At this stage, you can stop or slow down the pathological process without the help of drugs (diet, exercise). The patient may feel:
- discomfort in neck and shoulder muscles, their tension, stiffness;
- slight pain when turning or bending;
- infrequent and low-intensity headaches (most often appear after static or strenuous work, nervous experiences).
Stage 2. The height of the intervertebral discs decreases, compression of the nerve endings occurs, so severe pain appears in the neck, especially when making movements and turns. Muscle spasm disrupts the blood supply to the skull, so the symptoms associated with vascular insufficiency are added. The man notes:
- creaking in neck joints when dizzy;
- decreased visual acuity;
- tinnitus;
- dizziness;
- frequent headaches for no reason;
- numbness of the face and neck, loss of sensitivity in the skin of the hands and neck;
- shooting pains radiating to the shoulder blade;
- sleep disorders.
Stage 3. A herniated disc is formed (its core protrudes into the spinal canal), which causes disturbances in the work of the nervous system. Symptoms may include:
- numbness of the hands, paralysis of the upper limbs is possible;
- pain affects the entire neck area and can spread to the heart area;
- "floaters" appear in the eyes, nausea and vomiting;
- a lump in the throat or pain like a sore throat;
- the skin on the upper part of the body may not be felt at all;
- dizziness occurs with almost any movement;
- headaches are migraine in nature.
Stage 4. It is characterized by complete destruction of the disc:
- tinnitus may be constant;
- dizziness may be accompanied by loss of consciousness;
- As the blood supply to the cerebellar region of the brain decreases, coordination disorders appear.
Single intervertebral discs are very rarely affected. Usually the process involves the entire department. The destruction of individual disks can be in different stages.
Diagnostics
The diagnosis of cervical osteochondrosis includes instrumental examinations and evaluation of the complex of symptoms.
Basic information from instrumental methods will be provided by:
- x-ray - will show changes in the structure of the spine, but in the advanced stages of the pathology;
- computed tomography - shows changes in the vertebrae, but it is difficult to distinguish intervertebral tears and compression of the spinal cord;
- magnetic resonance imaging - allows to see intervertebral tears and their growth direction;
- Ultrasound duplex scan - shows the speed of blood flow in the area of suspected osteochondrosis.
When making a diagnosis, the doctor relies on the syndrome that manifests itself in the patient. A syndrome is a combination of symptoms of a disorder.
The following syndromes can develop with cervical osteochondrosis:
Vertebral- indicates that the pathological process involves bone and cartilage tissue. Manifestations:
- limited neck mobility;
- pain when turning the neck;
- structural changes in the vertebra or intervertebral disc (shown by x-ray).
Vertebral artery syndrome- means that the vertebral artery, which supplies the brain with blood, is involved in the pathological process. Main symptoms:
due to lack of blood flow:
- noise in the ears;
- dizziness;
- nausea and vomiting;
- pressure increases;
due to irritation of the nerve endings of the artery:
- severe headache (migraine);
- numbness of the skin on the scalp;
- "floaters" in the eyes or temporary blindness;
due to oxygen starvation;
- fainting;
- lethargy;
- loss of ability to focus on anything;
- depression;
- panic attacks.
Heart.Symptoms similar to problems with the cardiovascular system:
- pain in the sternum (sometimes as a burning sensation);
- shortness of breath and fatigue;
- acceleration of heart rate.
Koreshkovy.Depending on the damage of a certain pair of roots innervating the cervical region, it is related to the violation of the conduction of nerve impulses:
- 1-2 pairs of roots - pain or numbness in the back of the head;
- 3rd pair - numbness of the tongue, difficulty in chewing food;
- 4th pair - pain in the collarbone, swelling in the throat, difficulty in swallowing food;
- 5th pair – difficulty moving the arms with the problem concentrated in the shoulder region;
- 6th pair - discomfort in the area of shoulder blades and forearms;
- 7th pair - numbness of the hands, especially the middle and index fingers;
- 8th pair - numbness of the ring and little fingers.
Treatment options
Only an integrated approach is used in the treatment of osteochondrosis. The fight against pathology can even last for many years.
Drug therapy
The use of drugs for cervical osteochondrosis is aimed at:
- relieve pain;
- eliminate inflammation and swelling;
- reduce muscle tension in the neck area;
- improve blood circulation;
- protecting cartilage tissue from destruction and promoting its regeneration.
You should contact a neurologist for the diagnosis and treatment of cervical osteochondrosis. If the clinic has a vertebrologist who deals directly with diseases of the spine, you can contact him immediately.
Your doctor may prescribe the following medications:
- Non-steroidal anti-inflammatory drugs - relieve inflammation and swelling, reduce pain.
- B vitamins - help to improve the work of nerve tissue.
- Chondroprotectors - protect cartilage tissue from destruction and restore its structure.
- Medicines that improve blood flow.
- Muscle relaxants are drugs that relieve muscle spasms.
Physiotherapy methods
Physiotherapy methods can quickly alleviate the patient's condition and are combined with drugs:
- Electrophoresis– exposure of the affected area to a low-intensity electric current. Delivers medicinal substances directly to the problem area. It is usually prescribed with anesthesia to relieve pain or with a drug to improve blood flow to the cervical region.
- Ultrasound- has anti-inflammatory properties, improves blood circulation and metabolic processes.
- Magnetotherapy- helps to quickly remove tissue swelling and improve metabolic processes.
- Laser therapy– helps to improve blood circulation in the affected area, and also has an anti-inflammatory effect.

Massage
During drug treatment and physiotherapeutic treatment, it is better to undergo neck-collar massage from a specialist.
Self-massage can be used only very carefully, without trying to duplicate the depth of effect shown by a professional massage therapist in the future.

When performing the procedure, the specialist uses classic massage techniques:
- stroke - activates the surface layers of the skin;
- tightening - connects the deep layers of the skin;
- rubbing - warms and relaxes muscles, improves blood circulation;
- kneading - affects very deep tissues, so it is used carefully;
- vibration - tapping and shaking that completes the procedure.
Manual therapy
Sometimes with cervical osteochondrosis, it is recommended to consult a chiropractor. But this technique causes conflicting opinions: in some cases it certainly helps, and in others it almost makes it worse. Here's the whole point:
- There is no doubt that a chiropractor should be a highly qualified physician with medical training and specialties such as a neurologist or orthopedic traumatologist.
- Manual therapy for cervical osteochondrosis has many contraindications. Two people with similar symptoms may have different answers about the need for manual therapy - one can and should, and the other absolutely cannot.
There should be no strict indications and contraindications for contacting a chiropractor. They are determined by the attending physician and a direction is given for this type of therapy.
A highly qualified chiropractor will not work with a patient without studying the results of the X-ray.
Treatment at home
Traditional treatment prescriptions or the use of any home treatment should be discussed with the doctor in advance, because in each specific case they can either help or worsen the condition.
This applies, for example, to the needle applicator used. It consists of plastic spikes attached to a wide tape, a person applies to the painful area (you can lie on them). Thorns cause irritation of skin receptors and increase local blood circulation. However, it cannot be used for infectious and vascular diseases.
It is also popular to warm the diseased area with a mustard plaster or salt or sandbag. But with vascular diseases, this can also be dangerous.
Therapeutic exercise (physical therapy)
Therapeutic exercises are the safest method of treating cervical osteochondrosis. It is recommended to do this both in the period of exacerbation and in the future - to prevent the disease.
The patient should not feel pain while performing the exercises. Doing it "with pain" not only will not benefit, but can harm your health.
The simplest, but most effective movements are turns, bends and head rotations. It is strictly forbidden to do it at high speed and amplitude. Movements should be less noticeable. Despite such low mobility, exercise provides blood flow and improves its circulation in the neck area.
Lucky collar
The Shants collar is a rigid head support that relieves neck muscle tension and prevents movements that can cause pain. It is recommended to wear both during treatment and for the prevention of cervical osteochondrosis.
The collar is permanently worn. The vertebrae are fixed in the correct position and do not put pressure on each other, as well as on blood vessels and nerve endings. As a result, pain disappears, blood circulation normalizes, and many symptoms of pathology disappear.

If 5-7 cervical vertebrae are unstable, the bandage cannot be used, because it will not be possible to secure it in the correct position. It is also not recommended to wear a collar when the thyroid gland is enlarged.
Application of orthopedic pillow
Very often, osteochondrosis is aggravated by compression of the cervical artery and nerve roots when sleeping on an uncomfortable pillow. Orthopedic pillow ensures an even horizontal position of the spine at night.
By itself, it will not cure osteochondrosis, but it will alleviate the condition, and it will also be a good measure to prevent the development of degenerative processes in the spine.
Prevention
There are simple rules that, if followed, will help prevent premature aging of the intervertebral discs:
- control the weight, the norm exceeding 10 kg creates a critical load on the entire spine;
- try not to lift or carry heavy objects;
- if you need to carry a heavy bag, hold it alternately in your right and left hand (or it is better to use a backpack that will distribute the load evenly over your entire back);
- every half hour of static work should be replaced with light exercises to relieve muscle tension and improve blood circulation;
- It is useful to do physical education and sports exercises, for example, swimming, but running, jumping and weightlifting are harmful to the spine;
- use an orthopedic mattress and pillow to sleep.
Osteochondrosis of the cervical spine can significantly worsen a person's quality of life. The disease can be treated at the initial stage, but even as it develops, performing a complex of daily exercises, observing the rules of prevention, massage and other measures prescribed by the doctor allow you to lead a comfortable life.
























